
Semaglutide medications — such as Ozempic, the popular diabetes drug — have been linked to a reduced risk of Alzheimer’s disease for certain groups.
A new study, which was led by researchers at Case Western Reserve University in Cleveland, Ohio, revealed that patients who were prescribed semaglutide had a "significantly lower risk" of developing Alzheimer’s compared to those taking other types of anti-diabetic medications, according to a press release.
The researchers analyzed three years of medical records for nearly one million type 2 diabetes patients in the U.S.
NEW ALZHEIMER’S RESEARCH REVEALS ‘QUIET’ PHASE OF THE DISEASE, BEFORE SYMPTOMS APPEAR
The findings were published in Alzheimer’s & Dementia: The Journal of the Alzheimer’s Association on Thursday.
"Our study provides promising real-world evidence suggesting that semaglutide could be beneficial in preventing or slowing down the development of AD," lead author and biomedical informatics professor Rong Xu told Fox News Digital.
"The underlying mechanisms remain unknown, and future mechanistic studies and clinical trials are necessary to confirm the effects."
ALZHEIMER’S DISEASE COULD BE SLOWED BY BOOSTING A CERTAIN PROTEIN IN THE BRAIN, RESEARCHERS SAY
Alzheimer’s is the seventh-leading cause of death in the U.S., according to the Centers for Disease Control and Prevention, taking around 120,000 lives each year.
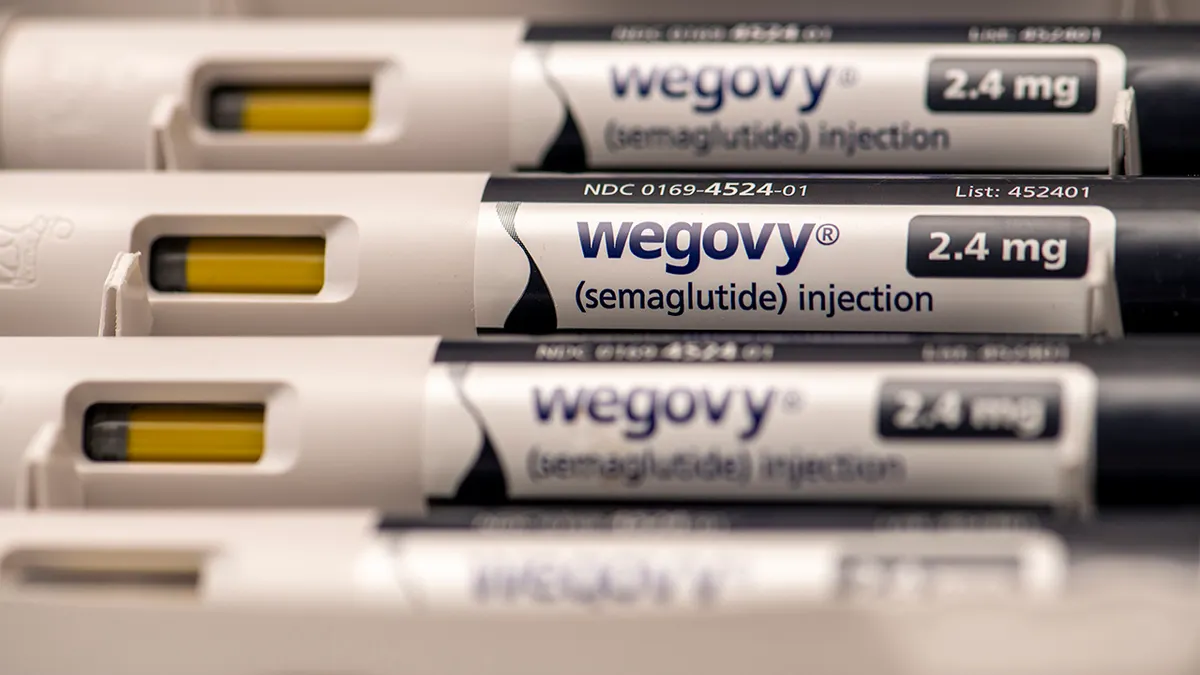
Semaglutide, the active ingredient in Novo Nordisk’s Ozempic, is a GLP-1 molecule that regulates blood sugar in diabetes patients.
It is also the active ingredient in Wegovy, Ozempic’s counterpart that is used to treat obesity.

The findings suggest that there could be potential beneficial effects of semaglutide in preventing or slowing down the development of Alzheimer’s in high-risk populations, such as patients with type 2 diabetes, Xu noted.
"This can provide some guidance in the choice of anti-diabetic medications for diabetes management and, at the same time, for preventing Alzheimer’s disease," she said.
MEAT CONSUMPTION LINKED TO HIGHER TYPE 2 DIABETES RISK IN OBSERVATIONAL STUDY
Dr. Sue Decotiis, MD, a New York City weight-loss doctor, said she was not surprised by the study’s discovery of the extra GLP-1 benefits.
"We know that GLP-1 drugs treat insulin resistance, which has a positive impact on the whole body – cardiovascular health, neurovascular health, decreased risk of stroke and better cognitive function," Decotiis, who was not involved in the research, told Fox News Digital.
Dr. Brett Osborn, a Florida neurosurgeon and longevity doctor who often prescribes Ozempic to his patients, said this study reinforces how metabolic health influences neurodegeneration.
"The connection becomes even more apparent when considering the links between obesity, chronic inflammation and conditions like Alzheimer’s disease, often referred to as ‘type 3 diabetes’ due to its association with insulin resistance in the brain," Osborn, who also was not involved in Case Western's research, told Fox News Digital.
In people with diabetes, a byproduct of insulin resistance is an increase in inflammation, Osborn noted, which is a "key driver" of neurodegeneration and cognitive decline.
"This suggests that effective management of insulin resistance and systemic inflammation reduction may be pivotal in slowing or preventing neurodegenerative diseases," he said.
Osborn agrees that the preventive effects of GLP-1 drugs will likely extend across various conditions.
"These drugs will ultimately be employed not just for diabetes, but as preventative and therapeutic agents for nearly all non-infectious age-related diseases, as well as conditions like alcoholism and drug addiction," he said.

While the study doesn’t claim that GLP-1s are a cure for Alzheimer’s, Osborn said, "It shifts the paradigm by addressing the underlying risk factors for Alzheimer’s rather than just its symptoms."
"It suggests a more comprehensive approach — one that tackles insulin resistance, obesity and inflammation," he went on.
By improving insulin sensitivity and reducing inflammation, these medications could provide direct benefits for not only the brain, but the entire body, he suggested.
"After all, most age-related conditions share common underpinnings and vary only by which part of the body is affected," Osborn said. "It’s simply a matter of geography."

Decotiis said she expects to see "more and more widespread benefits" from using this category of drugs, but that more studies are needed to prove that they slow the progression of Alzheimer’s.
"There needs to be a clear indication from the FDA to use these drugs for Alzheimer’s specifically in order for them to be covered by insurance," she added.
Xu reiterated that these findings "cannot be used to justify off-label prescription of semaglutide for Alzheimer’s disease prevention and treatment."
"For this to happen, randomized clinical trials are necessary," she said.
TO SIGN UP FOR OUR HEALTH NEWSLETTER
The researcher also acknowledged that the study had some limitations.
"This is a retrospective cohort study with inherent limitations related to uncontrolled or unmeasured confounding and biases," she said.

"Further research into semaglutide’s use will need to be further investigated through randomized clinical trials so alternative drugs can be tested as potential treatment for this debilitating illness."
The study received funding from the National Institute on Aging and the National Center for Advancing Translational Sciences.
For more Health articles, visit www.foxnews.com/health
When contacted by Fox News Digital, Ozempic maker Novo Nordisk issued the following statement.
"Novo Nordisk welcomes independent research investigating the safety, efficacy and clinical utility of our products."
A company spokesperson also stated that Novo Nordisk is conducting its own research into the effectiveness of oral semaglutide in early Alzheimer’s disease, with expected completion in 2025.