Aging brings two opposing trends in cancer risk: first, the risk climbs in our 60s and 70s, as decades of genetic mutations build up in our bodies. But then, past the age of around 80, the risk drops again – and a new study may explain a key reason why.
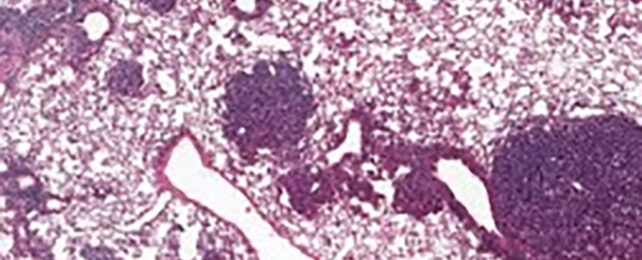
The international team of scientists behind the study analyzed lung cancer in mice, tracking the behavior of alveolar type 2 (AT2) stem cells. These cells are crucial for lung regeneration, and are also where many lung cancers get started.
What emerged was higher levels of a protein called NUPR1 in the older mice. This caused cells to act as if they were deficient in iron, which in turn limited their regeneration rates – putting restrictions on both healthy growth and cancerous tumors.

"The aging cells actually have more iron, but for reasons we don't yet fully understand, they function like they don't have enough," says cancer biologist Xueqian Zhuang, from the Memorial Sloan Kettering Cancer Center (MSK) in New York.
"Aging cells lose their capacity for renewal and therefore for the runaway growth that happens in cancer."
The same processes were found to be happening in human cells too: more NUPR1 leads to a drop in the amount of iron available to cells. When NUPR1 was artificially lowered or iron was artificially increased, cell growth capabilities were boosted again.
That potentially gives researchers a way of exploring treatments that target iron metabolism – especially in older people. It could perhaps restore lung capacity in those experiencing long-term effects from COVID-19, for example.
These findings also have implications for cancer treatments based on a type of cell death called ferroptosis, which is triggered by iron. This cell death is less common in older cells, the researchers found, because of their functional iron deficiency.
This perhaps also makes them more resistant to cancer treatments based on ferroptosis that are in development– so the earlier a ferroptosis treatment can be tried, the better it's likely to work.
"What our data suggests in terms of cancer prevention is that the events that occur when we're young are probably much more dangerous than the events that occur later," says cancer biologist Tuomas Tammela, from MSK.
"So, preventing young people from smoking, or from tanning, or from other obvious carcinogenic exposures are probably even more important than we thought."
There's lots more to explore here about the effects of NUPR1 and how it relates to stem cell function – both healthy regeneration and cancerous growth – but these are important findings for fighting cancer at any stage of life.
As always with cancer treatments, multiple factors need to be taken into account: the type and stage of cancer, other medical conditions that might be involved, and (as this new study shows) the age of the individual. The more personalized we can make these treatments, the more effective they can be.
"There's still a lot that's unknown about how aging actually changes the biology of cancer," says Zhuang.
The research has been published in Nature.