
If you find yourself sniffling at the merest hint of an irritant, you likely have a different set of microbes calling your nostrils home than everyone else. An international team of researchers has found a unique assortment of fungi up the noses of people who suffer from hayfever and asthma.
Hayfever, or allergic rhinitis, and asthma are two of the most common chronic airway conditions in Western countries. Globally, hayfever impacts more than 400 million people and asthma affects about 260 million.
To investigate potential causes, George Washington University computational biologist Marcos Pérez-Losada and colleagues sequenced nasal samples from 339 children and young people. That included 47 individuals with allergic rhinitis, 155 with both allergic rhinitis and asthma, 12 with just asthma, and 125 healthy controls.
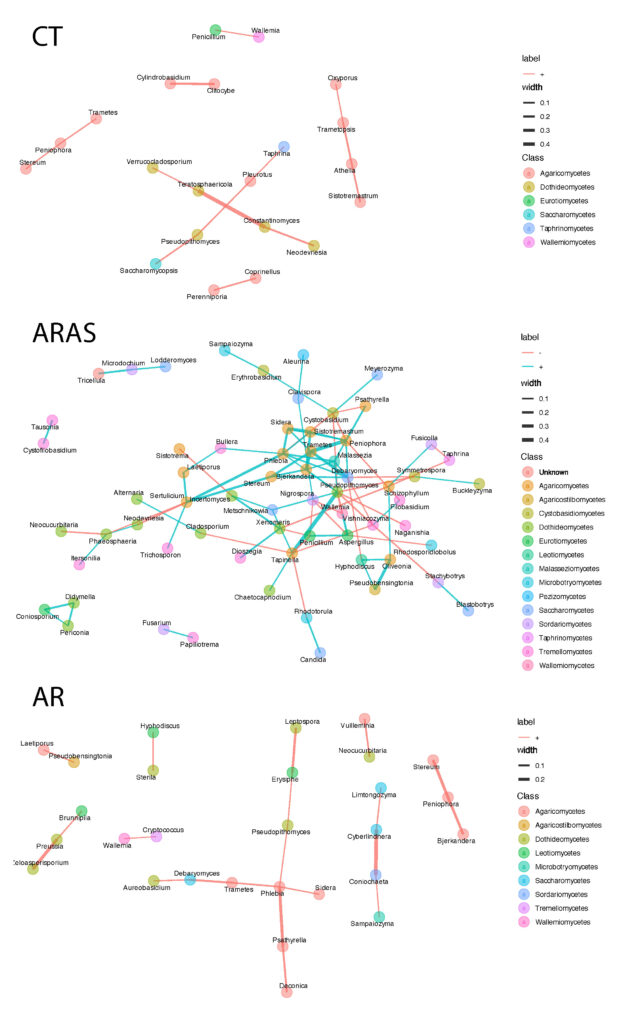
The researchers found those with allergic rhinitis, both with and without asthma, shared unique nasal microbiome features that differed from healthy individuals. The volunteers with one or both respiratory diseases had more diverse and abundant fungi populations in their nostrils.
"We showed that allergic rhinitis samples displayed a significantly higher fungal diversity and a different fungal community structure compared to those of healthy controls," says Luís Delgado, immunologist at Portugal's University of Porto. "This may suggest that allergic rhinitis increases the diversity and changes the composition of the upper airway's microbiome."
This mirrors the same patterns already known with bacteria, where opportunistic species are more prevalent in people with airway conditions. It also suggests the fungi may help alter our nose's immune system, the team suspects.
In the noses of people with both respiratory issues, members of the fungal populations had strikingly more ecological interactions than those in the control group or with allergic rhinitis alone. This supports previous research that suggested rhinitis alone and rhinitis with comorbid asthma may represent two distinct diseases.
The opportunistic species the researchers detected in greater abundance include Malassezia, which contributes to dandruff and acne; Aspergillus, a known allergy trigger; Candida, infamous for causing thrush; and Penicillium of antibiotic-producing fame.
"Among these dominant genera we detected common fungi that have been recognized in humans as allergenic or opportunistic pathogenic fungi," says Delgado. "This suggests that the nasal cavity is a major reservoir for fungi that could be involved in allergic rhinitis and asthma."
The team also compared the metabolites between the different samples as well, to see if they could hone in on some mechanisms behind these diseases. Differences in metabolic pathways between the healthy controls and those with airway conditions included more activity around the creation of the 5-aminoimidazole ribonucleotide molecule.
This substance has previously been associated with inflammatory bowel disease and colorectal cancers when elevated in the gut.
But to figure out if the disease is causing the fungal changes or the fungi are driving the disease, or both, these microbiome changes would need to be observed over time, the researchers caution.
"We could not control all patient-specific variables, such as disease severity and related treatment levels, and patients were sampled at a single time," Delgado explains. "Addressing some of these clinical variables would be interesting follow-ups of our study, if we could get the appropriate funding."
This research was published in Frontiers in Microbiology.